Maxillofacial Treatment
Apex Maxillofacial & Dental Hospital - Dental Clinic has been a part of the local community. Our desire for you to have the most comfortable dental experience available has motivated us to implement the latest technology into our practice from the waiting room to the dentist’s chair. We also offer wheelchair access & facilities. Apex Maxillofacial & Dental Hospital - Dental Clinic provides a relaxing environment with the full range of dental technology & training. We are the specialists & therefore do not need to waste your time referring you to other surgeries. All you do is sit back, relax & then enjoy your beautiful new smile.
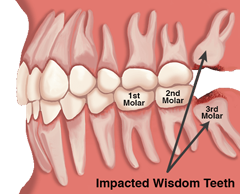
- WISDOM TOOTH REMOVAL
Why is wisdom tooth removal necessary?
 Some of us are unaffected by them, others develop painful conditions that require
their immediate removal. It is not always a wise decision to keep your wisdom teeth.
Find out why they may need to be removed, & where to find them in your mouth.
Some of us are unaffected by them, others develop painful conditions that require
their immediate removal. It is not always a wise decision to keep your wisdom teeth.
Find out why they may need to be removed, & where to find them in your mouth.Why are wisdom teeth removed?
- They are erupting in to an abnormal position, such as tilted, sideways or twisted.
- They are trapped below the gum line due to lack of space.
- An infection has developed from trapped food, plaque & bacteria, known as pericoronitis.
- The way the patients teeth bite together has changed, causing misalignment of the jaws.
- The erupted wisdom tooth lacks proper hygiene, because it is hard to reach, resulting in tooth decay.
How are wisdom teeth removed? (Painless Way) :
- After any elected methods of sedation have started to take effect, the Dr. Brijesh S Patel M.D.S. will start the procedure by:
- Numbing the tooth & tissues in the area of the mouth, where the wisdom teeth are located, with local anesthetic.At Brij Dental we Use Ultra Thin Needles & Instrument From Septodent France For Painless Anaesthesia.
- Any tissue & bone that is covering the tooth will be removed with the HITECH surgical instruments.
- Extraction instruments are used to loosen the tooth from any connective tissue in the tooth's socket.
- Once the tooth is loose enough, the Dr. Brijesh S Patel M.D.S.removes it with dental forceps.
- It may be necessary for the dentist to use stitches to close the tissue to aide in the healing process. Follow all of the instructions after surgery for a full recovery.
- JAW FRACTURES TREATMENT
Jaw Surgeries
 An oral surgeon is a specialist who has an expertise in performing surgeries related
to teeth,mouth & structures adjoining it.Here is brief description of some common
dental/oral surgeries performed by our expert oral surgeon.
An oral surgeon is a specialist who has an expertise in performing surgeries related
to teeth,mouth & structures adjoining it.Here is brief description of some common
dental/oral surgeries performed by our expert oral surgeon.Pre Prosthetic Surgeries:
Performed in the upper/lower jaws to facilitate wearing of dentures,crown & bridges,Implants.This includes alveoplasty(smoothening of bony ridges where dentures are going to seat),vestibuloplasty (deepening of vestibules to increase the surface area of bony ridges),removal of tori (bony nodules in the jaws).
Frenectomy:
Removal of a tissue flap below the upper lip in the mouth if it is too much prominent creating problem in dentures or is responsible for the space in between upper two front teeth.
Apicoectomy:
Removal of small cyst(infected tissue in the bone over the tooth root).
Crown Lengthening:
Increasing the height of the tooth which is too short to support the crown.
Incision & Drainage:
Removal of puss/infection from a swollen jaw/gum by puncturing/cutting the skin & draining it.
Removal of Impacted(Wisdom) Teeth:
It can be mostly an upper or lower third molar or a canine tooth which is buried in the bone & needs to be surgically removed.
Advanced oral surgical procedures:
- Removal of big cysts & tumours in the jaws which is usually done under general anesthesia in an operation theatre setup.
- Jaw joint(TMJ) surgeries:like TM joint ankylosis,subluxation,dis location.
- Fixing Jaw fractures & facial cuts due to trauma from accidents ,sports injury, violence.
- Trigeminal neuralgia surgeries.
- Implant surgeries:sinus lift,nerve repositioning,ridge augmentation.
- Closure of oro antral fistula:Simple flaps,Caldwell luc operation.
- Cosmetic surgeries of face & correction of jaw deformities
- ORAL CYSTS
What are Oral Cysts?
 Several forms or types of cysts may develop in the mouth cavity. Oral cysts are
also called dental cysts, as well as periapical, odontogenic or radicular cysts.
Dental cysts are a very common form of an odontogenic cysts. In most cases, such
cysts are caused by infections that result in the pulp or inner portion of the tooth
becoming infected & causing resultant decay, as well as the development of fluid
filled sacs or inflamed tissue. Fluids contained within such as sacs or cysts may
be sterile or infected. If not treated, infectious fluids may be reabsorbed &
spread infection to other locations in the body.
Several forms or types of cysts may develop in the mouth cavity. Oral cysts are
also called dental cysts, as well as periapical, odontogenic or radicular cysts.
Dental cysts are a very common form of an odontogenic cysts. In most cases, such
cysts are caused by infections that result in the pulp or inner portion of the tooth
becoming infected & causing resultant decay, as well as the development of fluid
filled sacs or inflamed tissue. Fluids contained within such as sacs or cysts may
be sterile or infected. If not treated, infectious fluids may be reabsorbed &
spread infection to other locations in the body.Types of Oral Cysts
- Periapical cyst- also known as a radicular cyst, these are the most common of odontogenic cyst types. The tooth becomes infected, leading to death of pulp tissues. Infected matter & toxins may escape through the apex (bottommost portion) of the tooth, leading to infection of surrounding tissues as well as the development of cysts caused by skin or gum tissue caused by lack of adequate blood supply.
- Keratocyst- This cyst is often difficult to diagnose, & results pertaining to content must rely on laboratory tests. They are rather aggressive & can be tricky to remove, as the cyst can grow into bone formations of the jaw.
- Dentigerous cyst - this type of cyst is the second most common, & develops within a dental follicle in close proximity to or surrounding an unerupted tooth. These type of cysts are commonly found around the third molars. These cysts can grow & alter positioning of teeth, but most do not cause symptoms or pain & often go unnoticed.
- Primordial cyst - this type of cyst develops instead of a tooth & is one of the rare forms of oral cysts.
Common Treatment for Cyst Removal (Cyst Operations)
The most common & beneficial treatment for cysts is excision or removal of the cyst. Before removing the cyst, the dentist or oral surgeon generally performs a biopsy, which involves the removal of a small portion or piece of tissue from the questionable cyst. The tissue sample is then sent to a laboratory where examination & analysis will be performed.
Cysts in mouth commonly form around the wisdom teeth, around impacted wisdom teeth, & in the pulp of teeth, & while the cyst itself might be benign, or harmless, dentists & oral surgeons most frequently suggest their removal before surrounding tissues or bone structures are damaged.
Cyst operations are generally performed under local anesthesia meaning the patient is awake during the procedure. In most cases, cysts are removed quickly & efficiently in under an hour. Large cysts a require more detailed or extensive surgery, which may or may not require bone reconstruction.
Who Benefits from Cyst Operations?
Anyone who has noticed or been diagnosed with a cyst in any portion of the oral cavity will benefit from its removal. If left untreated, cysts may cause ensuing infection or spread of infection to surrounding teeth, gum, or other mouth tissues. For other types of dental treatments, check out Placidway search.
- ORAL CANCERS & TUMOR DIAGNOSIS
Tumors diagnosis
 An important decision you will make about your cancer treatment is choosing a doctor,
a team & a cancer center that has the expertise to treat your cancer. As you
learn about your cancer diagnosis & treatment options, ask your doctor how soon
you need to make a treatment decision. You may seek a second or even third opinion.
Being able to talk openly & feel comfortable with your doctor, nurse, social
worker, & other office or health care team staff is important. Here are some
questions to consider asking as you choose your team:
An important decision you will make about your cancer treatment is choosing a doctor,
a team & a cancer center that has the expertise to treat your cancer. As you
learn about your cancer diagnosis & treatment options, ask your doctor how soon
you need to make a treatment decision. You may seek a second or even third opinion.
Being able to talk openly & feel comfortable with your doctor, nurse, social
worker, & other office or health care team staff is important. Here are some
questions to consider asking as you choose your team:About your cancer diagnosis:
- What type of cancer do I have?
- What stage is my cancer? What does that mean?
- What symptoms of cancer might I experience?
- What other types of tests will I need?
- Where can I get a second opinion?
Oral Cancers
Oral cancer treatment may include surgery, radiation therapy, or chemotherapy. Some patients have a combination of treatments.
At any stage of disease, people with oral cancer may have treatment to control pain & other symptoms, to relieve the side effects of therapy, & to ease emotional & practical problems. This kind of treatment is called supportive care, symptom management, or palliative care.
- REMOVAL OF COMLICATED TEETH
Removal of Complicated teeth
 Your dentist or oral surgeon might provide you a local anesthetic to numb the location
where the tooth will be removed. A more powerful, general anesthetic may be used,
especially if several of your teeth have to be eliminated at the same time. A general
anesthetic prevents pain in the entire body & will make you groggy or rest through
the procedure.
Your dentist or oral surgeon might provide you a local anesthetic to numb the location
where the tooth will be removed. A more powerful, general anesthetic may be used,
especially if several of your teeth have to be eliminated at the same time. A general
anesthetic prevents pain in the entire body & will make you groggy or rest through
the procedure.After removing the tooth, the dental professional or specialist may put in stitches (sutures) & location gauze over the wound to assist stop bleeding.
- JOINT SURGERY OF JAW BONES
Joint surgery of jaw bones
 TMJ total joint replacement systems are artificial orthopedic devices & are
used to replace a part of the body that has become painful, compromised &/ or
no longer functions properly. In orthopedic terms, TMJ prosthetics are considered
ball-&-socket joints that are made of 2 parts, the fossa & the condyle.
TMJ total joint replacement systems are artificial orthopedic devices & are
used to replace a part of the body that has become painful, compromised &/ or
no longer functions properly. In orthopedic terms, TMJ prosthetics are considered
ball-&-socket joints that are made of 2 parts, the fossa & the condyle.The fossa or socket part of the joint sits between the maxilla & the zygomatic process & is located next to your ear canal. Medical grade plastics are used to create this portion of the anatomy.
The condyle or ball protrudes from mandible’s structure extending to the fossa to complete the joint. Hard metals are used in the construction to make the implant last longer.
- LIMITED MOUTH OPENING(OSMF)TREATMENT
Limited Mouth Opening (OSMF) Treatment
 Oral submucous fibrosis (OSMF) is an insidious chronic disease affecting any part
of the oral cavity & sometimes the pharynx. Although occasionally preceded by
& or associated with vesicle formation, it is always associated with juxtaepithelial
inflammatory reaction followed by a fibroelastic change of the lamina propria, with
epithelial atrophy leading to stiffness of the oral mucosa, causing trismus &
inability to eat . OSMF has a high rate of morbidity because it causes progressive
inability to open the mouth, resulting in inability to eat & consequent nutritional
deficiencies. Mortality rate is significant because it transforms into oral cancer,
particularly squamous cell carcinoma at a rate of 30% .
Oral submucous fibrosis (OSMF) is an insidious chronic disease affecting any part
of the oral cavity & sometimes the pharynx. Although occasionally preceded by
& or associated with vesicle formation, it is always associated with juxtaepithelial
inflammatory reaction followed by a fibroelastic change of the lamina propria, with
epithelial atrophy leading to stiffness of the oral mucosa, causing trismus &
inability to eat . OSMF has a high rate of morbidity because it causes progressive
inability to open the mouth, resulting in inability to eat & consequent nutritional
deficiencies. Mortality rate is significant because it transforms into oral cancer,
particularly squamous cell carcinoma at a rate of 30% .Management includes cessation of habit & surgical release of fibrous bands followed by forceful opening of the mouth by coronoidectomy & coverage of surgical defects with nasolabial flap & postoperative active jaw physiotherapy for 6 months . Surgery may induce scar tissue which reduces mouth opening due to scar contraction in mouth closing muscles . Relapse is a common complication that occurs after surgical release of the oral trismus caused by OSMF. A variety of jaw opening devices have been used to treat trismus .
The purpose of this paper is to report a definite treatment approach that combines surgery with active physiotherapy to improve the jaw opening & to prevent relapse. Small effort has been made in the present study aiming to endure adequate, functional disease free mouth opening & to detect any developing malignant change at its earliest.
- CORRECTIVE JAW SURGERY
Corrective Jaw Surgery
 Corrective jaw, or orthognathic surgery is performed by an oral & maxillofacial
surgeon (OMS) to correct a wide range of minor & major skeletal & dental
irregularities, including the misalignment of jaws & teeth. Surgery can improve
chewing, speaking & breathing. While the patient's appearance may be dramatically
enhanced as a result of their surgery, orthognathic surgery is performed to correct
functional problems.
Corrective jaw, or orthognathic surgery is performed by an oral & maxillofacial
surgeon (OMS) to correct a wide range of minor & major skeletal & dental
irregularities, including the misalignment of jaws & teeth. Surgery can improve
chewing, speaking & breathing. While the patient's appearance may be dramatically
enhanced as a result of their surgery, orthognathic surgery is performed to correct
functional problems.- Difficulty chewing, or biting food
- Difficulty swallowing
- Chronic jaw or jaw joint (TMJ) pain & headache
- Excessive wear of the teeth
- Open bite (space between the upper & lower teeth when the mouth is closed)
- Unbalanced facial appearance from the front, or side
- Facial injury
- Birth defects
- Receding lower jaw & chin
- Protruding jaw
- Inability to make the lips meet without straining
- Chronic mouth breathing
- Sleep apnea (breathing problems when sleeping, including snoring)
- RIDGE CORRECTION(PRE PROSTHETIC SURGERIES)
Ridge Correction
 Prosthetics is the replacement of missing teeth (lost or congenitally absent) &
contiguous oral & maxillofacial tissues, with artificial substitute. Now ,there
remains significant number of patients, who can never be made to use dentures effectively,
because of - - Bone atrophy - Soft tissue hypertrophy - or localized soft &
hard tissue problems. In these patients pre-prosthetic surgery offers significant
contribution by removing hindrance for prosthesis stability & retention.
Prosthetics is the replacement of missing teeth (lost or congenitally absent) &
contiguous oral & maxillofacial tissues, with artificial substitute. Now ,there
remains significant number of patients, who can never be made to use dentures effectively,
because of - - Bone atrophy - Soft tissue hypertrophy - or localized soft &
hard tissue problems. In these patients pre-prosthetic surgery offers significant
contribution by removing hindrance for prosthesis stability & retention.
Pre-prosthetic surgery
Pre-prosthetic surgery Pre-prosthetic surgery is carried out to reform/redesign soft/hard tissues, by eliminating biological hindrances to receive comfortable & stable prosthesis. Preprosthetic surgery is defined as surgical procedures designed to facilitate fabrication of a prosthesis or to improve the prognosis of prosthodontic care.
Aims of pre-prosthetic surgery:
Aims of pre-prosthetic surgery Provide adequate bony tissue support for the placement of RPD/CD/IMPLANTS. Provide adequate soft tissue support, optimal vestibular depth. Elimination of pre-existing bony deformities e.g. tori , prominent mylohyoid ridge, genial tubercle. Correction of maxillary & mandibular ridge relationship. Elimination of pre-existing soft tissue deformities, e.g. epulis , flabby ridges, hyperplastic tissues. Relocation of mental nerve. Etc.
- ORAL & FACIAL CLEFT SURGERIES
Causes
 Early in pregnancy, all babies have an opening in the lip & palate. As the baby
grows, these openings should gradually grow together. By birth, the openings should
be closed. For some reason, in children with oral-facial clefts, these openings
fail to close. The exact reason these openings do not close is not known.
Early in pregnancy, all babies have an opening in the lip & palate. As the baby
grows, these openings should gradually grow together. By birth, the openings should
be closed. For some reason, in children with oral-facial clefts, these openings
fail to close. The exact reason these openings do not close is not known.Risk Factors
Oral-facial clefts are more common in males. Other factors in the infant that may increase the chance of oral-facial clefts include:
- Having other birth defects
- Having a sibling, parent, or other close relative born with an oral-facial cleft
Factors in the mother during pregnancy that may increase the chance of oral-facial clefts include
- Taking certain medications, such as antiseizure drugs, thalidomide, or retinoic acid
- Smoking
- Consuming alcohol
- Having diabetes
Treatment
Surgery is the main treatment. The primary goal of surgery is to close the gap in the lip & palate. Other surgery may also be needed for:
- Bite alignment surgery if the jaw is not aligned properly
- Plastic &/or nasal surgery to improve facial appearance & function
A cleft defect can make it difficult for your child to eat or drink. Your child may be given a dental plate, which is placed in the roof of the mouth. It should make it easier to eat & drink until surgery can be done.
Cleft palates may also be associated with ear & hearing problems. If your child has a middle ear infection or fluid build-up, your doctor may recommend:
- Medications to treat infection or prevent fluid build-up
- Surgery to drain built-up fluid & prevent future infections
Hearing testing should be done regularly. Rarely, children with cleft palate may benefit from hearing aids.
- TRIGEMINAL NURALGIA
What Is Trigeminal Neuralgia?
 Trigeminal neuralgia (TN), also called tic douloureux, is a condition that is characterized
by intermittent, shooting pain in the face. Trigeminal neuralgia affects the trigeminal
nerve, one of the largest nerves in the head. The trigeminal nerve sends impulses
of touch, pain, pressure, & temperature to the brain from the face, jaw, gums,
forehead, & around the eyes.
Trigeminal neuralgia (TN), also called tic douloureux, is a condition that is characterized
by intermittent, shooting pain in the face. Trigeminal neuralgia affects the trigeminal
nerve, one of the largest nerves in the head. The trigeminal nerve sends impulses
of touch, pain, pressure, & temperature to the brain from the face, jaw, gums,
forehead, & around the eyes.Trigeminal Neuralgia
Medication can provide relief from pain & reduce the number of attacks. The first form of treatment is typically anti-seizure medications, which are drugs that block nerve firing. Some other second line or adjunctive medications include muscle relaxants & tricyclic antidepressants..
- MPDS DIAGNOSIS & TREATMENT
What Is MPDS Diagnosis?
 Myofacial Pain Dysfunction Syndrome is a disease that disturbs the muscles which
help in chewing. It is characterized by pain & limited movement of the TMJ (Temporomandibular
joint).
Myofacial Pain Dysfunction Syndrome is a disease that disturbs the muscles which
help in chewing. It is characterized by pain & limited movement of the TMJ (Temporomandibular
joint).Temporomandibular joint (TMJ) also known as the craniomandibular joint & is peculiar to mammals. It is a bilateral (both sides) joint or articulation between the temporal bone (bone near the temple region of the head) & mandible (lower jaw). This joint lies in front of or adjacent to the ear & helps in opening & closing of the mouth by permitting movement of the mandible or the lower jaw.
Temporomandibular joint is covered by muscles of mastication which helps in chewing or mastication. Major muscles of mastication include:
- Temporalis
- Masseter
- Lateral pterygoid
- Medial pterygoid
Other muscles assist these muscles of mastication in doing its function.
Myofacial Pain Dysfunction Syndrome (MPDS) is a pain disorder in which unilateral (one side) pain is referred from the trigger points in myofacial structures (muscles of the face) to the muscles of the head & the neck. Pain is constant & dull in nature, but the pain may range from mild to intolerable.
MPDS is more common in females in the age group of 15 to 40 years as compared to the males.
- LASER SURGERIES
Laser surgeries
 Laser
surgery is incredibly versatile & plays an important role in a growing number
of common procedures. Though laser surgery is most notably associated with cosmetic
treatments, it is equally effective for preventative purposes.
Laser
surgery is incredibly versatile & plays an important role in a growing number
of common procedures. Though laser surgery is most notably associated with cosmetic
treatments, it is equally effective for preventative purposes.Here are some of the ways that lasers can be used:
- Reshaping soft tissue Lasers can remove soft tissue to expose more of the natural tooth (crown lengthening), reshape soft tissue to make gummy smiles more attractive, & remove uncomfortable soft tissue folds caused by denture wear.
- Frenectomy Lasers can improve speech & the feeding habits of babies, children & adults by untying the tongue.
- Tumor removal When benign tumors have formed in the soft tissue areas of the mouth, a laser can completely remove them without causing pain.
- Biopsy Lasers are sometimes used to perform a biopsy on suspicious areas of soft tissue. This biopsy procedure can be performed instantly & with great precision.
- Apthous Ulcer treatment
How are laser procedures performed?
Different types of laser have been created to treat different conditions. Each laser uses a different wavelength of light, which predicates its best use. The most common types of laser are carbon dioxide lasers & diode lasers, which are usually employed to treat soft tissue problems. The surgeon will decide which type of laser is best to use after conducting X-rays & a thorough examination.
The laser beam is extremely bright, & special glasses will be provided to protect the eyes.
The surgeon will then direct the beam at the affected area & carefully remove the soft tissue & treat the indicated area
The procedure will take far less time than conventional methods, & cause far less anxiety & discomfort.
If you have questions or concerns about laser surgery, please ask your Oral & Maxillofacial Surgeon.
- COSMETIC SURGERIES & SCAR REVESIONS
What is scar revision surgery?
 Scar revision surgery is meant to minimize the scar so that it is more consistent
with your surrounding skin tone & texture.
Scar revision surgery is meant to minimize the scar so that it is more consistent
with your surrounding skin tone & texture.Scars are visible signs that remain after a wound has healed. They are unavoidable results of injury or surgery, & their development can be unpredictable. Poor healing may contribute to scars that are obvious, unsightly or disfiguring. Even a wound that heals well can result in a scar that affects your appearance. Scars may be raised or recessed, different in color or texture from surrounding healthy tissue or particularly noticeable due to their size, shape or location.
Your treatment options may vary based on the type & degree of scarring & can include:
- Simple topical treatments, such as bioCorneum+
- Minimally invasive procedures
- Surgical revision with advanced techniques in wound closure
Although scar revision can provide a more pleasing cosmetic result or improve a scar that has healed poorly, a scar cannot be completely erased.
- EARLOBE CORRECTIONS
What is scar revision surgery?
 Have your ear lobe repair (Lobuloplasty) procedure at The London Cosmetic Clinic,
by our highly experienced cosmetic doctors.
Have your ear lobe repair (Lobuloplasty) procedure at The London Cosmetic Clinic,
by our highly experienced cosmetic doctors.The earlobe is the lower, fleshy part of the ear that is sometimes pierced. The area consists of a delicate piece of skin that is made up of fat & skin. A split earlobe is more likely to occur for those that wear heavy earrings constantly.
Elongation of the hole or complete splitting of the earlobe can occur either over time through the thin wire of an earing being pulled by the weight of an earring or through trauma such as the jewellery being yanked or snagged suddenly. It is natural for the hole which the jewellery hangs through to stretch slightly over time if the earrings worn are heavy but would only be described as a split earlobe if the jewellery pulls right through the skin of the lobe causing the tissue to be in two pieces.
Big holes in the earlobe from big plug earrings that stretch the hole intentionally can also be repaired. We also complete ear lobe reduction procedure to re-shape & re-size the fleshy lobe part of the ear.
- CHEILOPLASTY
Cheiloplasty
 Lip reduction also known as cheiloplasty is a surgical procedure for reducing the
size of the lip & also to correct the abnormally shaped lip. Large lips in some
people look beautiful. Whereas in certain people, it will look vice versa. Certain
natural conditions may cause fat lips. Fat, luscious lips can be sexy in some people.
But, some others may find it displeasing & out of proportion with the rest of
the face. You can change your lip-size to your desired comfort level & balance
the look.
Lip reduction also known as cheiloplasty is a surgical procedure for reducing the
size of the lip & also to correct the abnormally shaped lip. Large lips in some
people look beautiful. Whereas in certain people, it will look vice versa. Certain
natural conditions may cause fat lips. Fat, luscious lips can be sexy in some people.
But, some others may find it displeasing & out of proportion with the rest of
the face. You can change your lip-size to your desired comfort level & balance
the look.
The procedure starts with a general or local anesthesia. Lip reduction surgery takes about an hour to complete. An incision will be made inside the mouth in the length of a lip. A strip of skin or tissue from one lip or both will be removed through the incision. The surgeon will enhance the shape of the mouth & lip while sustaining a natural look. The incision will be closed with dissolvable sutures. According to your preferences, the surgeon will modify the curves around the lips.
There can be slight swelling & bruising around the surgical area. It will dissolve after a few days of surgery. The surgery will describe you the dos & don’t s after the procedure. Proper care is suggested in order to prevent infection & other risks. The healing time may depend upon the person’s bodily ability to heal. Final results will be visible in about three months after surgery. You will be able to resume your normal activities within few days after the surgery.
- NASAL BRIDGE CONNECTIONS
Nasal bridge corrections
 A nose which looks beautiful on one person will not necessarily look good on another
person. Attempts are made to keep the nose in conformity & harmony with the
rest of the face, keeping in mind the necessary specific changes which the patient
came to us for.
A nose which looks beautiful on one person will not necessarily look good on another
person. Attempts are made to keep the nose in conformity & harmony with the
rest of the face, keeping in mind the necessary specific changes which the patient
came to us for.Many patients feel that the change in shape will be so much that it might be the subject of discussion amongst family & friends. But, in reality neither the patient nor the patients / friends really remember the original shape of the nose a few weeks after surgery.
The operation takes anywhere from 1 ½ to 3 hours for the procedure, depending on what has to be done. Patients can go home the same day.
Anaesthesia:
The operation can be done done under local anesthesia plus sedation or general anaesthesia.
Procedure:
The incisions for closed rhinoplasty are usually made inside the nose. The nasal skin is lifted away from the cartilage & bones. Then the necessary modifications to the skeleton (bones & cartilages) are made. The excess skin redrapes itself onto the new framework & shrinks over a period of time.
Since rhinoplasty involves correction the framework or scaffolding over which the skin drapes, the results may vary according to the skin type of the patient too. Hence, caucasians have better results than asians & asians have better results than africans. Similarly women have better results than men.
Sometimes if the chin is smaller or disproportionate as compared to the nose or the face as a whole chin enlargement might be needed, which can be performed simultaneously to bring the face into proper balance.
- GUM SURGERIES & FLAP SURGERY
Gum surgeries
 When recession of the gingiva occurs, the body loses a natural defense against both
bacterial penetration & trauma. When gum recession is a problem, gum reconstruction
using grafting techniques is an option.
When recession of the gingiva occurs, the body loses a natural defense against both
bacterial penetration & trauma. When gum recession is a problem, gum reconstruction
using grafting techniques is an option.When there is only minor recession, some healthy gingiva often remains & protects the tooth, so that no treatment other than modifying home care practices is necessary. However, when recession reaches the mucosa, the first line of defense against bacterial penetration is lost.
In addition, gum recession often results in root sensitivity to hot & cold foods as well as an unsightly appearance of the gum & tooth. When significant, gum recession can predispose to worsening recession & expose the root surface, which is softer than enamel, leading to root caries & root gouging.
- SINUS LIFTING SURGERIES
What is sinus lift surgery?
 A
sinus lift procedure is a surgery that adds bone height to the upper jaw in the
area of molars & premolars. It is also sometimes called as sinus augmentation.
Bone graft is added between the jaw & the maxillary sinuses, which are on either
side of the nose. To make room for the bone, the sinus membrane is moved upward,
or "lifted." A sinus lift is done by an oral & maxillofacial surgeon.
A
sinus lift procedure is a surgery that adds bone height to the upper jaw in the
area of molars & premolars. It is also sometimes called as sinus augmentation.
Bone graft is added between the jaw & the maxillary sinuses, which are on either
side of the nose. To make room for the bone, the sinus membrane is moved upward,
or "lifted." A sinus lift is done by an oral & maxillofacial surgeon.
Reasons for inadequate bone in upper molar area
When patients who have lost teeth in upper jaw, desire fixed teeth on dental implants; they find that they have lost a lot of amount of bone which was vital for anchoring teeth implants. There are several reasons for loss of bone volume below the maxillary sinus.
- The maxillary sinus keeps expanding with age & soon patients have little bone left above the 2nd premolar, 1st molar & 2nd molar.
- Bone loss due gum disease.
- Once teeth are gone, bone begins to be resorbed. If teeth have been missing for a long time, then a lot of bone is lost.
- HARD & SOFT TISSUE AUGMENTATION-BONE GRAFTING
Bone remodeling & choice of graft material
 Bone remodeling is a very complex & crucial component
of the hard tissue augmentation process. The bone remodeling would use the triad
of cell, scaffold, & signaling molecule to achieve bone regeneration. The primary
cell type targeted are the osteoblasts; however, unless the bone graft scaffold
that is provided is completely degraded, the space cannot be filled up with vital
bone. Another issue that can come up with a bone graft scaffold is the potential
effect(s) that the degradation products can have on the formation of new bone. The
key is to have the optimum graft resorption time. This, in other words, is when
a graft that stays long enough to provide the necessary physical support for osteoblast
migration & bone growth but which resorbs & does not interfere with continued
bone growth. Depending on the clinical situation, the clinician would choose a graft
material with varying resorption times.
Bone remodeling is a very complex & crucial component
of the hard tissue augmentation process. The bone remodeling would use the triad
of cell, scaffold, & signaling molecule to achieve bone regeneration. The primary
cell type targeted are the osteoblasts; however, unless the bone graft scaffold
that is provided is completely degraded, the space cannot be filled up with vital
bone. Another issue that can come up with a bone graft scaffold is the potential
effect(s) that the degradation products can have on the formation of new bone. The
key is to have the optimum graft resorption time. This, in other words, is when
a graft that stays long enough to provide the necessary physical support for osteoblast
migration & bone growth but which resorbs & does not interfere with continued
bone growth. Depending on the clinical situation, the clinician would choose a graft
material with varying resorption times.
Type of bone grafts
- Autograft
- Xenograft
- Allograft
